Syringes and Needles for Injection, Types, Use, etc, FAQ
Syringe and Needle to Inject in Medical and Other Fields
A syringe is a simple piston
pump consisting of a piston (although in modern syringes it is a plunger) that
fits snugly into a cylindrical tube called a barrel. The plunger can be pulled
linearly and pushed into the tube, allowing the syringe to enter and expel the
liquid or gas through the discharge port at the front (open) end of the tube.
The open end of the syringe can be connected to a hypodermic needle, syringe,
or tubing to direct flow in and out of the cylinder. Syringes are commonly used
in clinical medicine to administer injections, infuse intravenous therapy into
the bloodstream, apply compounds such as glue or lubricant, and collect/measure
fluids. The word "syringe" is derived from the Greek σύριγξ (syrinx,
meaning "pan flute", "tube").
Definitions of Syringe
§ A device consisting of a nozzle of various
lengths and a squeezable rubber flask and used for injection or irrigation
§ A gravity device
consisting of a reservoir attached to a long rubber tube ending in a
replaceable nozzle used for vaginal or bowel irrigation.
§ An instrument (for example, for
injecting drugs or collecting body fluids) consisting of a hollow cylinder
attached to a piston and a hollow needle
§ A medical device that is used to
inject fluid into, or withdraw fluid from, the body. A medical syringe consists
of a needle attached to a hollow cylinder that is fitted with a sliding
plunger. The downward movement of the plunger injects fluid; upward movement
withdraws fluid. Medical syringes were once made of metal or glass, and
required cleaning and sterilization before they could be used again. Now most
syringes used in medicine are plastic and disposable.
What is hypodermic needle?
A hypodermic (hypo - under, dermal - skin) needle is a hollow
needle that is often used with a syringe to inject substances into the body or
to extract fluids from the body. It can also be used to collect fluid samples
from the body, such as taking blood from a vein by venipuncture. Large-bore
subcutaneous intervention is particularly useful in the treatment of catastrophic
blood loss or shock.
The hypodermic needle also ensures rapid delivery of fluids.
It is also used when an injectable substance cannot be taken orally because it
is not absorbed, like insulin, or because it damages the liver.
Hypodermic needles also play an important role in research that requires sterile conditions.
A hypodermic needle reduces contamination during sterile substrate inoculation in two ways:
i. its surface is extremely smooth, which prevents airborne pathogens from being trapped between the surface irregularities of the needle, which can later be transferred to the medium as contamination.
ii. The needle tip is extremely sharp, which can
reduce the diameter of the remaining hole after the membrane is broken, thereby
preventing microbes larger than the hole from contaminating the substrate.
What are medical syringes?
The threads of the Luer lock tip of this 12mL disposable
syringe keep it securely connected to a tube or other apparatus.
Syringe usually made entirely of glass, with no parts made
from metal, nor any other material.
What is antique glass and metal syringe?
The syringes and needles market sector includes disposable
and safety syringes, injection pens, needleless injectors, insulin pumps and
specialty needles.
Syringes are used with injection needles to inject fluids or
gases into body tissues or to remove them from the body. Injecting air into a
vein is dangerous because it can cause an air embolism.
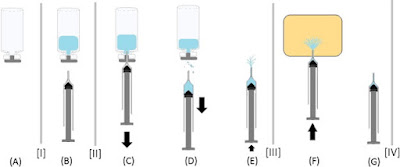
Prevention of embolism by removing air from the syringe is
one of the reasons for the familiar image of holding the syringe up, tapping
and releasing a small amount of fluid before injecting blood flow.
The syringe barrel is made of plastic or glass, usually has
graduated markings to indicate the amount of liquid in the syringe, and is
almost always transparent. Glass syringes can be sterilized in an autoclave.
Plastic syringes can be two- or three-piece. The three-piece
syringe contains a plastic piston/rubber-tipped plunger to create a seal
between the piston and cylinder, while the two-piece syringe is designed to fit
perfectly between the plastic piston and cylinder around the seal without the
need for a separate synthetic rubber piston.
Two-piece syringes are traditionally used in European
countries to avoid the introduction of additional materials, such as silicone
oil, which are required to lubricate the three-piece piston.
Most modern medical syringes are plastic because they can be
cheaply thrown away after one use, reducing the risk of spreading blood-borne
diseases.
The reuse of needles and syringes has caused the spread of
diseases, especially HIV and hepatitis, among drug users.
Syringes are also often reused by diabetics because they can
go through several daily insulin injections several times a day, which has
become a problem that many can afford. Even if only one person uses the syringe
and needle, the procedure is still dangerous because it can carry bacteria from
the skin into the bloodstream, causing serious and sometimes fatal infections.
In the medical
environment, disposable needles and syringes effectively reduce the risk of
cross-contamination.
Medical syringes are sometimes used without needles to orally
administer liquid medicine to small children or animals, or milk to small
animals, because the dose can be accurately measured and it is easier to inject
the medicine into the mouth than the test object. drink from a measuring cup.
What type Tip Designs of Syringes exist?
Syringes have different designs for the area where the blade
fits into the body of the syringe. Perhaps the most famous of these is the Luer
lock, which simply twists the two together.
Bodies with small, simple joints are known as sliding tips
and are used when the syringe is attached to something that does not have a
screw lock mechanism.
Similar is the catheter tip, which is a sliding tip, but
longer and tapered, so it's good for pushing into things where a plastic cone
would fit tightly. It can also be used to wash wounds or large abscesses in
veterinary use.
There is also an eccentric tip, where the nozzle at the end
of the syringe is not in the center of the syringe, but to the side. This is
why the blade attached to the syringe is roughly in line with the walls of the
syringe itself, and is used when the blade needs to be very close to parallel
to the skin (for example, to inject a superficial vein or artery).
What are multipoint needle syringes?
There are syringes designed to be refilled from a built-in tank (container) after each injection, so they can perform multiple or multiple injections in one refill. It is rarely used in human medicine due to the risk of cross-infection with needles.
Exceptions are the personal insulin
auto-injector used by patients with diabetes and dual-chamber syringes designed
to administer pre-filled saline flush after medication.
What are Standard U-100 insulin syringes?
Insulin syringes are marked with "units" of
insulin.
Syringes for insulin users are designed for standard U-100
insulin. The dilution of insulin is such that 1 ml of liquid insulin contains
100 basic "units" of insulin.
Because insulin vials are usually 10 mL, each vial contains
1,000 units.
Insulin syringes are specially made for self-injection and
have friendly features:
• finer needles for less pain
• Shorter needles because the insulin injection is
subcutaneous (under the skin) instead of intramuscular
• Markings on insulin units to facilitate drawing a measured
dose of insulin and
• Clear the dead space to reduce complications caused by
incorrect monitoring of symptoms of different insulin strengths. Size and
designation of the U-100 syringe
What are venom extraction syringes?
Venom extraction syringes differ from standard syringes because they usually do not penetrate the wound. The most common types have a plastic mouthpiece placed over the affected area and then the plunger of the syringe is retracted, creating a vacuum that supposedly draws in the venom.
Attempts to treat a snakebite in this manner are expressly discouraged as they
are ineffective and may cause further damage.
Syringes of this type are sometimes used to remove botfly
larvae from the skin.
What are dose-sparing syringes?
A dose-sparing syringe and needle being used to draw up a
Covid-19 vaccine
A dose-sparing syringe is one which minimises the amount of
liquid remaining in the barrel after the plunger has been depressed.
These syringes feature a combined needle and syringe, and a
protrusion on the face of the plunger to expel liquid from the needle hub.
Such syringes were particularly popular during the COVID-19
pandemic as vaccines were in short supply.
What are oral syringes?
An oral syringe is a measuring device which doctors use to
accurately measure doses of liquid medication, expressed in milliliters (ml).
This type of syringe does not have threaded points, as there is no need to
insert a needle or other instrument.
The contents of this syringe are simply sprayed or sucked
from a syringe directly into the mouth of a person or animal.
Oral syringes come in a variety of sizes ranging from 1 to 10 mL and larger. The most commonly
used sizes are 1 ml, 2.5 ml and 5 ml in hospitals and clinics.
What are dental syringes?
A toothpick is used by dentists to inject anesthesia. It
consists of a capped syringe attached to a sealed cartridge containing
anesthetic solution.
In 1928, Bayer Dental developed, developed and manufactured a
closed cartridge system under the registered trademark Carpule®. The current
owner of the trademark is Kulzer Dental GmbH.
Carpels have long been reserved for anesthetics for dental
use. It's practically a bottomless bottle.
This is replaced by an elastomer plug that can be inserted
into the body of the cartridge.
This stopper will be pushed into the plunger of the syringe.
The neck is closed with a rubber cap.
The dentist inserts the cartridge directly into a stainless
steel syringe that has a double (disposable) needle. A tip located on the side
of the container breaks the capsule and the plunger pushes the product. Thus,
the product does not come into contact with the surrounding air during use.
An accessory tool (usually part of a dentist) used to deliver
water, compressed air, or a mist (created by combining water and compressed
air) into the oral cavity for the purpose of rinsing (removing debris from the
area being worked on) dentist . ), also known as a dental syringe or dental
irrigation nozzle.
The three-way syringe/nozzle has separate internal channels
that deliver air, water or a mist created by combining compressed air with a
stream of water. The syringe tip can be separated from the main body and
replaced if necessary.
In the UK and Ireland, hand syringes are used to inject
lidocaine into patients' gums.
Syringe Regulation
In some jurisdictions, the sale or possession of hypodermic
syringes may be controlled or prohibited without a prescription by an
authorized professional, due to its suspected use with illegal intravenous
drugs.
What are some Non-medical Uses of Syringes?
Syringes have many non-medical applications like:
- Recreation
- Injecting liquid or fluid into any object, etc.
What are laboratory applications of syringes?
Laboratory grease, often used to lubricate burrs and
stopcocks, is sometimes filled into syringes for ease of use.
Some chemical compounds such as thermal paste and various
adhesives, e.g. epoxy, sold in prepackaged syringes.
Disposable medical syringes are often used in research
laboratories for their convenience and low cost.
Another application is to use the tip of a needle to add fluids to confined spaces, such as washing some scientific equipment.
It is often used for measuring and transferring solvents and reagents where high accuracy is not required. On the other hand, microliter syringes can be used to measure and dispense chemicals very accurately using a small diameter capillary like the barrel of the syringe.
The polyethylene construction of these disposable syringes usually makes them relatively chemically resistant.
However, there is a risk
that the contents of the syringes will leach plasticizers from the syringe
material. Where this is a problem, non-disposable glass syringes may be
preferred.
Glass syringes may also be preferred where a high level of
precision is important (ie, quantitative chemical analysis) because their
engineering tolerances are lower and the plungers operate more smoothly. In
these applications, pathogen transmission is usually not a problem.
Syringes used with a long needle or cannula are also useful for transferring fluids through rubber septa when oxygen or atmospheric moisture is excluded. Examples include switching to air-sensitive or pyrophoric agents such as phenylmagnesium bromide and n-butyllithium. Glass syringes are also used to inject small samples for gas chromatography (1 μl) and mass spectrometry (10 μl).
Injection drivers can also be used with syringes in cooking
Another use of syringes in cooking is to inject liquids (such
as sauce) into other foods or to make certain sweets.
Syringes can also be used when cooking meat to improve flavor
and texture by injecting juices into the meat, and when cooking to inject
fillings into baked goods. Typically, these syringes are made of stainless
steel components, including the barrel. This facilitates easy disassembly and
cleaning.
Other Uses
Syringes are used to fill ink cartridges with ink in fountain
pens. Common shop applications include injecting adhesive into tight spaces to
repair joints where disassembly is impractical or impossible; and inject
lubricants into work surfaces without spillage.
Sometimes a large syringe without a needle is used for very
small farmed mammals.
Historically, large pumps that used a reciprocating motion to
pump water were called syringes. Bombs of this type are used as fire
extinguishers.
There are fountain syringes where the liquid is in a bag or
can and goes through a tube into the syringe. In earlier times, enema syringes
were used for this.
Loose snus is often consumed using one's own syringes. The
mouthpiece is removed so that the opening is the width of the room. Snus can be
tightly packed in the chamber and fall over the upper lip. Syringes, called
slicers, are also made for this specific purpose.
Blunt needle assemblies are useful for industrial and non-medical applications
The blunt needle assembly provides many useful applications in both industrial and non-medical applications. The types of needles used in these types of establishments are usually not sterile because the processes in which they are used do not require sterile needles.
A blunt tip is often
preferred over a sharp tip as it helps reduce the risk of accidents such as
puncturing the skin. The flat tip also helps prevent damage to other materials
in the areas where it is used. For example, needles may be part of your ink
cartridge filling processes. You want to make sure the needle fills the
cartridge but is not sharp enough to go through the plastic chambers where the
ink is in the cartridge.
Do arts and crafts companies use blunt needle assemblies to make products?
Small businesses that make their own arts and crafts products
by hand often use blunt needle sets. Common applications include the use of
needles to apply glues, paints and adhesives. Needle assemblies are designed
for use with corded bottles such as syringes. Needle size, like wall thickness,
determines how effective glues, paints, and pipe glues are. Depending on the
types of products you make, you can use different gauge sizes and wall
thicknesses. You can also use custom and secondary processes in situations
where you have specific requirements. Another option you can consider to get
different dispensing needles is to get them in lab kits.
History of Syringes Development
De Medicina
by the Roman author Aulus Cornelius Celsus, later the first medical textbook to
be printed
• Piston syringes were used in ancient
times. During the 1st century AD Aulus Cornelius Celsus mentioned the use of
them to treat medical complications in his De Medicina.
• 9th century: The Iraqi/Egyptian
surgeon Ammar ibn 'Ali al-Mawsili' created a syringe in the 9th century using a
hollow glass tube, and suction to remove cataracts from patients' eyes, a
practice that remained in use until at least the 13th century.
• Pre-Columbian Native Americans created
early hypodermic needles and syringes using "hollow bird bones and small
animal bladders".[33][34]
• 1650: Blaise Pascal invented a syringe
(not necessarily hypodermic) as an application of what is now called Pascal's
law.
• 1844: Irish physician Francis Rynd
invented the hollow needle and used it to make the first recorded subcutaneous
injections, specifically a sedative to treat neuralgia.
• 1853: Charles Pravaz and Alexander Wood
independently developed medical syringes with a needle fine enough to pierce
the skin. Pravaz's syringe was made of silver and used a screw mechanism to
dispense fluids. Wood's syringe was made of glass, enabling its contents to be
seen and measured, and used a plunger to inject them. It is effectively the
syringe that is used today.
• 1865: Charles Hunter coined the term
"hypodermic", and developed an improvement to the syringe that locked
the needle into place so that it would not be ejected from the end of the
syringe when the plunger was depressed, and published research indicating that
injections of pain relief could be given anywhere in the body, not just in the
area of pain, and still be effective.
• 1867: The Medical and Chirurgical
Society of London investigated whether injected narcotics had a general effect
(as argued by Hunter) or whether they only worked locally (as argued by Wood).
After conducting animal tests and soliciting opinions from the wider medical
community, they firmly sided with Hunter.
• 1899: Letitia Mumford Geer patented a
syringe which could be operated with one hand and which could be used for
self-administered rectal injections.
• 1946: Chance Brothers in Smethwick,
West Midlands, England, produced the first all-glass syringe with
interchangeable barrel and plunger, thereby allowing mass-sterilisation of
components without the need for matching them.
• 1949: Australian inventor Charles
Rothauser created the world's first plastic, disposable hypodermic syringe at
his Adelaide factory.
• 1951: Rothauser produced the first
injection-moulded syringes made of polypropylene, a plastic that can be
heat-sterilised. Millions were made for Australian and export markets.
• 1956: New Zealand pharmacist and
inventor Colin Murdoch was granted New Zealand and Australian patents for a
disposable plastic syringe.
See also
• Fire syringe has two meanings:
o A fire piston, a fire starting device
o A squirt, in the form of a large
syringe, one of the first firefighting devices in history used to squirt water
onto the burning fuel.
• Autoinjector, a device to ease
injection, e.g. by the patient or other untrained personnel.
• Hippy Sippy
• Jet injector, injects without a
needle, by squirting the injection fluid so fast that it makes a hole in the
skin.
• Luer Taper, a standardized fitting
system used for making leak-free connections between syringe tips and needles.
• Needle exchange programme, is a social
policy based on the philosophy of harm reduction where injecting drug users
(IDUs) can obtain hypodermic needles and associated injection equipment at
little or no cost.
• Trypanophobia, a fairly common extreme
fear of hypodermic syringes
• Syrette, similar to a syringe except
that it has a closed flexible tube (like that used for toothpaste) instead of a
rigid tube and piston.
• Syringing the ear to remove excess ear
wax.
• Syrinx, the nymph from classical
mythology after which syringes were supposedly named.
• Safety syringe, with features to
prevent accidental needlesticks and reuse
• Vaginal syringe