Typhoid Meaning Etiology Pathogenesis
Typhoid Etiology and Pathogenesis
Meaning of Typhoid: Typhoid fever is an acute infectious disease caused by typhoid. The lesion is characterized by the proliferation of cells in the whole body monocyte macrophage system. The lesions in the lymphatic tissue at the terminal ileum were the most prominent. The main clinical manifestations are persistent fever, symptoms of neurotoxicity and gastrointestinal symptoms, relative slowness, splenomegaly, skin roseola and reduction of neutrophils and eosinophils. Sometimes serious complications such as intestinal bleeding and intestinal perforation can occur.
Etiology and pathogenesis
Group D in the genus Salmonella typhi, Gram-negative. Its
bacterial "O" antigen, flagella "H" antigen and
"Vi" antigen on the surface can cause the body to produce
corresponding antibodies, especially "O" and "H" antigens
are strong, so serum agglutination test (fat response), Widal Reaction) to
determine the increase in antibodies in serum, can be used as a basis for
clinical diagnosis of typhoid fever. Endotoxin released during bacterial lysis
is the main cause of disease.
Typhoids or carriers are the source of the disease. Bacteria
are excreted with feces and urine, contaminate food, drinking water, milk,
etc., or infect the alimentary canal through flies. It is more common in
children and young adults. Onset can occur throughout the year, with the most
in summer and autumn. After the illness, a relatively stable immunity can be
obtained, and rarely reinfected.
Typhoid bacteria are mostly destroyed in the stomach. Whether
or not the disease mainly depends on various factors such as the amount of
bacteria reaching the stomach.
When the amount of infected bacteria is large
(105), the bacteria can enter the small intestine through the small intestinal
mucosal epithelial cells and invade the lymphatic tissue of the intestinal
wall, especially the collective lymph nodes or solitary lymph nodes at the end
of the ileum. And along the lymphatic vessels to reach the mesenteric lymph
nodes.
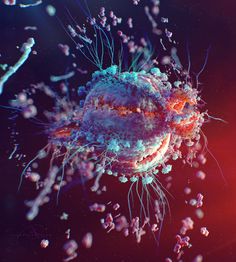
Typhoid bacteria in lymphoid tissues are engulfed by macrophages, grow
and reproduce in them, and can enter the blood through the chest duct, causing
bacteremia.
Bacteria in the blood are quickly swallowed by the cells of the
whole body mononuclear macrophage system, and multiply in them, causing
enlargement of the liver, spleen, and lymph nodes.
During this period, the
patient has no clinical symptoms, so it is called the incubation period, which
is about 10 days. Thereafter, as the bacteria multiply and the endotoxin is
released into the bloodstream again, the patient develops symptoms of sepsis
and toxemia.
Because a large amount of typhoid bacteria in the gallbladder
enters the intestine again with bile, it repeatedly invades the sensitized
lymphoid tissue, causing it to have a strong allergic reaction, causing
intestinal mucosal necrosis, shedding and ulcer formation.
Typhoid Pathological changes and clinicopathological connections
The inflammation caused by typhoid bacteria is an acute
proliferative inflammation characterized by macrophage proliferation. When
hyperplasia is active, typhoid bacteria, red blood cells, and cell debris are
phagocytosed in the macrophage cytoplasm, and the role of phagocytosis of red
blood cells is particularly obvious.
This macrophage is called typhoid. Typhoid
cells often aggregate into clusters and form small nodules called typhoid
granuloma or typhoid nodule. They are characteristic lesions of typhoid and
have pathological diagnostic value.
Typhoid granuloma
Intestinal lesions
Typhoid intestinal lesions are the most
common and obvious lesions in the lower ileum and solitary lymph nodes.
According to the development process of the disease, it is divided into four
stages, and each stage lasts about one week.
(1) Myeloid swelling period:
In the first week of onset, the
lymph tissue in the lower ileum is slightly swollen, bulging on the surface of
the mucosa, gray-red, soft. The surface of the raised tissue resembles the sulcus
of the brain, and the collective lymph nodes are most typical.
(2) Necrosis period
Occurred in the second week after the
onset of the disease, and local intestinal mucosal necrosis of the lesion was
caused by various reasons.
(3) Ulcer stage
ulcers are formed after the mucous membrane
of necrotic intestine is shed. The edge of the ulcer is raised and the bottom
is uneven. The major axis of ulcers in the collective lymph nodes is parallel
to the major axis of the intestine. The ulcers in the solitary lymph nodes are
small and round.
Ulcers are usually deep and submucosal, and severe necrosis
can reach the muscle layer and serosa layer, and even perforation, such as
invasion of small arteries, can cause severe bleeding. This period usually
occurs in the third week of onset.
(4) Healing period
This is equivalent to the fourth week of onset.
The granulation tissue of the ulcer filled it with hyperplasia, and the
epithelium of the edge of the ulcer regenerated and covered and healed.
Typhoid Intestinal Disease A: Myeloid swelling, B: Necrotic,
C: Ulcer
2, other lesions Mesenteric lymph nodes, liver, spleen and
bone marrow due to the activation of macrophages cause the corresponding
tissues and organs to enlarge. Microscopic examination showed typhoid granuloma
and focal necrosis.
Myocardial fibers may have edema or even necrosis, renal
tubular epithelial cells may have edema and pale red papules (roseola) appear on
the skin. Coagulation necrosis often occurs in the diaphragm, rectus abdominis
and adductor muscles transsexual).
Clinically, myalgia and skin irritation
occur. Most patients with typhoid fever have no obvious lesions in the
gallbladder, but typhoid bacteria can multiply in bile.
Even after the
patient's clinical recovery, the bacteria can still survive in the bile and be
excreted from the intestine through the bile.
They are still carriers in a
certain period of time, and some patients can even become chronic carriers or
carriers for life.
Typhoid patients may have complications such as intestinal
bleeding, intestinal perforation, and bronchial pneumonia. If there are no
complications, it usually heals in 4-5 weeks. Chronic infections can also
affect joints, bones, meninges and other areas.
Share on Social Media for Personal Safety and Professional Development of all >>